Introduction:
As of right now, what do you believe would be the most important health concern on your list? Heart conditions, don’t they? Any cardiac problem carries the danger of a heart attack, which is a serious medical emergency.
This happens when a portion of the heart muscle loses its blood supply, usually as a result of an arterial blockage nearby. Chest discomfort that may spread is one of the symptoms. There is a medical emergency that requires hospitalization.
This also known as myocardial infarction, is characterized by discomfort in the chest and other areas of the body, along with additional symptoms including perspiration, nausea, and dyspnea.
A person’s life may be saved if they can recognize the early warning signs of a heart attack and receive treatment quickly. Though they are both medical emergencies, this is not the same as cardiac arrest, which occurs when the heart stops beating completely. Heart arrest can result from a heart attack if care is not received. This page describes heart attack symptoms, causes, and available treatments.
Often referred to as a myocardial infarction, this condition occurs when the heart muscle doesn’t receive enough blood. The longer the cardiac muscle is left untreated to restore blood flow, the more damage it will sustain.
These are mostly caused by coronary artery disease (CAD). A severe coronary artery spasm, or abrupt contraction, is a less frequent reason that can cut off blood supply to the heart muscle.
The most prevalent indicator of this is chest discomfort. However, additional symptoms including nausea, lightheadedness, and dyspnea may also occur. Symptoms vary from person to person and can be either severe or moderate. Some folks could be completely unaware of any heart attack warning symptoms.
We shall examine the causes, symptoms, risk factors, diagnosis, and treatment of heart attacks in further detail in this article.
What Is A Heart Attack?
This disorder, which occurs when there is insufficient blood supply to certain cardiac muscles, is exceedingly harmful. A blockage in one or more of your heart’s arteries is typically the reason for this lack of blood flow, however, there are other possible causes as well.
The damaged heart muscle will start to perish without blood supply. If blood flow is not restored promptly, a heart attack may result in death or irreversible cardiac damage.
This emergency poses a serious risk to life. Call 911 if you believe you or the person you are with is experiencing a heart attack. Even a few minutes of delay might cause death or irreversible cardiac damage.
When blood flow to the heart is interrupted or obstructed, this occurs. Damage may result to the afflicted area if the heart is not receiving enough oxygen-rich blood. The heart muscle starts to perish as a result.
You run the danger of developing heart failure and other severe consequences if your heart isn’t receiving the blood and oxygen it needs to work correctly.
This medical emergency is potentially fatal. The sooner you receive medical care that helps your heart’s blood flow return to normal, the higher your chances of recovery.
Usually, the accumulation of fatty deposits in the coronary arteries—which carry blood to the heart—causes this obstruction. Further obstructing blood flow, a blood clot may develop if the plaque bursts.
Insufficient blood flow can cause damage or death to the impacted heart muscle, which can result in major consequences including heart failure or even death. This can cause pain or discomfort in the chest, shortness of breath, nausea, dizziness, pain in the jaw, neck, arm, or back, and cold chills.
Prompt medical intervention is essential to limit cardiac damage and restore heart blood flow.
What Takes Place During A Heart Attack, Exactly?
Blood flow to a portion of the heart ceases or is significantly reduced during a heart attack, which damages or kills that area of the heart muscle. It can interfere with your heart’s ability to pump blood when a portion of it is dying from a lack of blood supply. Blood flow to the rest of your body may be reduced or stopped as a result, which might be fatal if left untreated.
The goal of treatment is to limit damage by restoring blood flow to the heart as soon as possible. This is often accomplished with drugs or surgery.
The plaque within an artery may occasionally burst or rupture. This causes the plaque’s underlying materials to become visible to the circulation, which in turn causes a blood clot to develop.
When the rupture occurs, the body’s natural clotting process starts. Blood platelets adhere to the broken plaque and release substances that cause the blood clot. Acute blockage is the term for when the clot is so big that it stops the blood flow through the artery.
The injured or dead heart muscle begins to develop if blood flow is not promptly restored. How long the blockage lasts and how much of the heart muscle is oxygen-deprived determine how severe the damage is.
Heart Attack Symptoms
- Chest Pain
Although it can come from different sources, chest discomfort is one of the most typical signs of a heart attack. In the case of a heart attack, chest discomfort usually has distinct features.
Physical activity, tension, or even rest can exacerbate the pain, which can range from mild to severe. Usually lasting a few minutes, it might come and go. These symptoms, which include tightness in the chest, an elevated heart rate, and trouble breathing, might be mistaken for heart attack symptoms.
Breathing deeply or moving around may exacerbate chest discomfort that is caused by strained muscles or inflammation in the ribs, muscles, or joints.
- Breath
One typical sign of a heart attack is shortness of breath, which can happen with or without chest pain or discomfort. The obstruction in the coronary arteries causes the heart muscle to get insufficient oxygen, which is why it occurs. This lowers the quantity of oxygen flowing to the lungs and the rest of the body by impairing the heart’s capacity to pump blood efficiently.
Shortness of breath is caused by a condition in which your hemoglobin or red blood cells are reduced, which lowers the quantity of oxygen that can be transported in your blood. When the heart is unable to pump blood effectively, fluid accumulates in the lungs, making breathing difficult.
- Indigestion
The term “indigestion” describes pain or discomfort in the chest or upper belly that usually occurs after eating. Even though it’s a frequent problem with many causes, indigestion can occasionally be a sign of a more serious illness, such as a heart attack.
Indigestion should be treated right once if it is accompanied by other worrisome symptoms, such as dizziness, breathing difficulties, or chest discomfort, as these might indicate a heart attack or other serious illness.
It’s best to be safe and have a medical expert check you out, even if you’re not sure if it’s indigestion or something more severe. This is because heart-related problems can be much improved by early treatment.
- Cold Sweats
Cold sweats may indicate a heart attack, especially if they are accompanied by additional symptoms including shortness of breath, nausea, dizziness, or pain spreading to the arms or jaw. Seek prompt medical assistance if you or someone else encounters these symptoms. It’s important to pay attention to cold sweats, particularly if they appear out of character or are accompanied by chest pain or other heart attack symptoms.
Consulting a healthcare practitioner is always advisable, even if the origin of the cold sweats is unknown. This is especially true if there are additional dangerous symptoms present.
- Dizziness
When dizziness is accompanied by additional symptoms, such as those mentioned above, it should be treated as a possible emergency since it might indicate many other health problems. Lives can be saved by early intervention, especially in cases of heart attacks or other cardiovascular catastrophes.
A heart attack that results in cardiogenic shock, in which the heart cannot pump enough blood to fulfill the body’s demands, can cause a sudden decrease in blood pressure. This can lead to lightheadedness, disorientation, or even fainting since the brain isn’t getting enough blood.
- Other Areas
Referred pain is the condition whereby pain after a heart attack radiates to other locations. It happens because of the connections between the body’s nerves. There are intimate connections between the nerves supplying the heart and those in the arms, neck, jaw, back, and stomach. The brain may perceive pain as originating from one of these other regions when the heart muscle undergoes ischemia.
- Fatigue
In addition to being a typical symptom of a heart attack, fatigue can also be a warning indication before one occurs. Exhaustion is a natural reaction to stress or physical effort, but excessive or unexplained exhaustion can be a serious symptom of a serious medical condition, such as cardiovascular problems.
Even in the absence of chest pain or other overt symptoms, fatigue may still be an indication that a heart attack is coming. Before a heart attack, people may feel lethargic or exhausted for a few days or weeks. The person may first reject this extended exhaustion as stress or fatigue since it may be modest. But it’s crucial to understand that chronic weariness, particularly if unfamiliar or unexplained, may be a sign of an underlying cardiac condition.
- Anxiety
Before, during, or after a heart attack, anxiety may strike. Feelings of anxiety or panic might result from the stress and dread of having a heart attack, particularly if the individual has a history of anxiety or panic episodes.
Seeking medical assistance right once is crucial if you have chest pain or discomfort combined with nausea, dizziness, shortness of breath, or any other heart attack symptoms. To rule out more serious problems, it is advisable to have a healthcare professional check you out, even if you think it could just be anxiety.
Some heart attacks, particularly in women, the elderly, and those with diabetes, may be “silent” or moderate, with no visible or severe symptoms. It’s critical to get medical attention right once any of these symptoms appear, even if they are minor or intermittent. Early medical attention can greatly lessen cardiac damage.
How Can One Experience A Heart Attack?
A lot of people have chest discomfort when they have a heart attack. Either crushing pain or a squeezing or weight sensation may be experienced. Beginning in the chest, it may progress to the left arm, shoulder, neck, jaw, back, or down toward the waist.
It’s common for people to mistakenly believe they have heartburn or indigestion rather than a heart attack. For some, the sole symptoms are sweating, nausea, or shortness of breath.
In an attempt to repair the wound, the body tries to create a blood clot at the location of the plaque rupture.
The clot may stop blood flow via the coronary artery entirely or in part. The heart muscle is deprived of oxygen and nutrients necessary for optimal function because of this obstruction.
This happens without the person showing any outward signs of illness. These are called silent heart attacks, and those with diabetes, the elderly, and people with a history of heart issues are more likely to experience them. Unbeknownst to the victim, silent heart attacks can cause irreversible damage to the heart muscle.
How Does A Heart Attack Happen?
A blockage in a blood artery supplying your heart is the most common cause of heart attacks. The most common cause of this is plaque, a sticky material that can accumulate inside your arteries. Atherosclerosis is the term for such accumulation. Coronary artery disease is the term used to describe the accumulation of atherosclerotic plaque in the blood vessels leading to the heart.
There are instances where plaque deposits inside the coronary arteries burst or break open, causing a blood clot to become lodged where the rupture occurred. This might result from the clot blocking the artery, which would prevent blood flow to the heart muscle.
Ruptures of the plaque can cause heart attacks, however, this is uncommon and only makes up 5% of all heart attacks. The following causes can result in this type of heart attack:
- Arterial spasm in the heart.
- Rare diseases, such as those that result in abnormal blood vessel narrowing.
- Injury that results in coronary artery rips or ruptures.
- Air bubble or blood clot that enters a coronary artery, for example, or obstruction that originated elsewhere in your body.
- Disorders of eating. These can harm your heart over time and eventually cause a heart attack.
- Abnormal heart arteries.
Other disorders can prevent your heart from getting enough blood for an extended amount of time, such as low blood pressure, low oxygen levels, or an accelerated heartbeat.
Risk Factors of Heart Attack

- Age and Sex
Both sex and age are significant determinants of heart attack risk, with distinct trends seen in men and women at different phases of life. It is more common for men to have a heart attack between the ages of 45 and 65. The protective effects of estrogen in women before menopause are partially to blame for this.
Heart attacks often occur in women ten years later than in males, typically between the ages of 55 and 65. The protective properties of estrogen, which support the maintenance of healthy blood arteries before menopause, are responsible for this. Following menopause, women’s risk of heart disease rises sharply and may even approach that of males.
If you have any heart attack symptoms, including chest pain, shortness of breath, dizziness, exhaustion, pain radiating to the arm or jaw, or cold sweats, you should get medical attention right once, regardless of your age or gender. In addition to saving lives, prompt medical intervention can lessen the severity of cardiac damage.
- Heart Disease
Heart disease is a general phrase used to describe a variety of disorders affecting the anatomy and function of the heart. It is one of the main causes of mortality globally and encompasses several illnesses.
Heartbeat irregularities are called arrhythmias. When the electrical impulses in the heart malfunction, the heart beats too quickly, too slowly, or irregularly. While some arrhythmias pose little threat, others might cause serious problems including cardiac failure or stroke.
Heart disease is a broad category of disorders affecting the heart and blood vessels. Age, sex, heredity, and lifestyle choices are risk factors for heart disease, however many types of heart disease may be avoided with lifestyle modifications, routine checkups, and early intervention. Over time, heart health may be improved and the chance of getting heart disease can be considerably decreased by controlling risk factors such as diabetes, high blood pressure, high cholesterol, and obesity.
- Lifestyle
A healthy lifestyle is essential for both managing and preventing heart disease. People’s risk of cardiovascular diseases, high blood pressure, heart attacks, and stroke can be considerably decreased by embracing heart-healthy behaviors. The following are important lifestyle modifications and elements that can support better heart health.
It might be simpler to maintain a heart-healthy lifestyle when you have a strong network of family, friends, or community organizations to offer emotional support and accountability. Encourage people to join you in adopting healthy habits, such as cooking meals or going on a walk to obtain exercise.
Keeping an eye on risk factors and modifying your health plan as necessary requires routine check-ups with your healthcare practitioner. Over time, little, sustained improvements can have a big impact on your heart health.
- Health Conditions
Numerous long-term medical disorders can have a major effect on cardiovascular health. The risk of heart disease can be decreased and general health can be improved by managing these diseases with medication, lifestyle modifications, and routine monitoring.
The severity of sleep apnea can be lessened by sleeping on your side, avoiding alcohol and sedatives before bed, and losing weight.
Surgery may occasionally be advised to remove extra tissue or address anatomical problems that are causing the disease. Reducing the risk of cardiac issues requires managing and controlling these illnesses. This article provides a summary of common heart-related illnesses, their effects on the heart, and management options.
What Issues Might Arise After A Heart Attack?
Among the complications linked to heart attacks are:
- An irregular heartbeat
- Heart failure.
- Cardiac valve issues.
- A stroke.
- Abrupt cardiac arrest.
- Anxiety and depression
- Cardiogenic shock
Heart attack-related mechanical issues, including a ruptured free wall or ventricular septal defect. If a heart attack is not treated right away, they are more likely to occur.
How Does One Feel During A Heart Attack?
When you are having a heart attack, you feel as though someone is putting a lot of pressure on your chest or that you are carrying a lot of weight on it. This ache can last for a while.
Additionally, you may begin to perspire a lot and feel weak, lightheaded, or as though you’re about to faint. You may occasionally get slight discomfort in your limbs, back, neck, or jaw as well. You may also experience breathing difficulties.
A vast array of emotional and physical feelings might be experienced by the person. There are several similar experiences and warning indications that people frequently report, albeit these symptoms might differ from person to person.
Someone can suffer a quiet heart attack in which they do not exhibit the usual symptoms. Rather, they could have no symptoms at all or only minor discomfort, but later on, they might have back pain, shortness of breath, or unexplained exhaustion. Those who have diabetes or are elderly are more likely to experience these.
Typical symptoms of a heart attack include dizziness, nausea, cold sweats, shortness of breath, chest discomfort, and occasionally pain that radiates to the jaw or arms. It might also be accompanied by a sense of dread or imminent disaster. It is crucial to pay attention to any unexpected or inexplicable discomfort, especially if it persists for more than a few minutes, as some people may have more mild or atypical signals, even while others may suffer normal symptoms. Get treatment right away if you or someone you’re with thinks they may be having a heart attack.
Heart Attack Facts
In addition to individuals designated male or female at birth, heart attacks can occur in both men and women. You can alter several risk factors, such as high blood pressure, high LDL (“bad”) cholesterol, diabetes, and smoking status, albeit they become more prevalent as you age.
You could hear some of the following terminology used when someone suffers a heart attack:
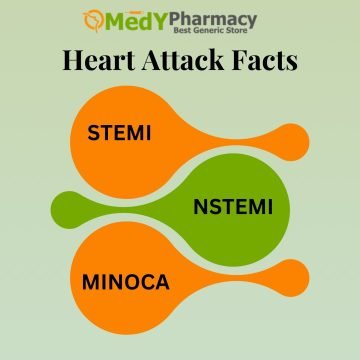
- STEMI
A cardiac attack in which the coronary arteries are occluded. To limit damage to the heart muscle and restore blood flow to the heart, it is deemed a medical emergency that has to be treated very quickly. The heart muscle sustains less damage the faster the heart’s blood flow is restored. The amount of cardiac muscle that is oxygen-deprived grows with each minute of delay, potentially causing irreversible harm.
A severe heart attack known as STEMI occurs when a coronary artery is completely blocked, seriously damaging the heart muscle. To restore blood flow and reduce damage, early treatment is essential, especially angioplasty or clot-busting drugs.
- NSTEMI
A coronary artery that is sufficiently constricted to significantly decrease blood flow but not completely blocked after a heart attack. If you suffer from symptoms such as nausea, dizziness, shortness of breath, or chest discomfort, you should get medical attention very once. The symptoms should be taken carefully and investigated by a healthcare professional, regardless of how minor or sporadic they are. Preventing more serious cardiac disease and saving lives are two benefits of early intervention.
Since the blockage is not total and less heart muscle is destroyed, the prognosis for NSTEMI is often better than for STEMI. It still involves the danger of consequences, though, such as heart failure, arrhythmias, and more heart attacks. The impacted cardiac muscle becomes injured as a result of the decreased oxygen. Tissue damage can still occur even if the damage is not as severe as in a STEMI.
- MINORCA
A heart attack in which the major coronary arteries show no signs of occlusion. When there is evidence of damage to the heart muscle but no substantial blockage or obstruction in the coronary arteries that would normally result in a heart attack, this condition is known as MINOCA. Traditional techniques of detecting heart attacks rely on finding blockages in coronary arteries, making this illness a little more uncommon and potentially challenging to diagnose.
When the underlying cause is found and treated properly, the prognosis for MINOCA is usually favorable. With the right care and adjustments to their lifestyle, many patients recover. To lower the danger of future heart issues, MINOCA must be continuously managed and monitored because it can occasionally be connected to other cardiovascular disorders.
Angina vs A Heart Attack
The term “angina” refers to chest discomfort that results from decreased blood supply to the heart muscle. It is a typical heart disease sign. Two primary forms of angina exist:
The most prevalent and predictable kind of angina is stable angina, which frequently happens during physical activity or stressful situations. In contrast, unstable angina is unpredictable and has to be treated as a medical emergency.
It can be difficult to distinguish angina from a heart attack in many situations, particularly when unstable angina is present. Angina attacks might feel similar to heart attacks.
A sudden, but brief, episode of chest discomfort may be mistaken for an angina attack if you have stable angina that flares up with exercise and goes away with rest. If your chest discomfort doesn’t go away when you rest or if it comes and goes for ten minutes or more, you could be suffering a heart attack.
Discussing angina management with your physician may help you better comprehend the distinction between angina and heart attack symptoms and prepare you if your chest pain is a heart attack sign.
What Should I Do in the Event of a Heart Attack?
You must receive prompt medical attention after a heart attack to clear the clogged artery and minimize damage. How much time do you have while having a heart attack? Treating a heart attack is best done within an hour or two of the onset of symptoms. You risk more heart damage and a shorter lifespan if you wait longer.
Chew a 325 mg aspirin as you wait for emergency personnel to come after calling. As a strong blood clot inhibitor, aspirin can reduce your risk of dying from a heart attack by 25%.
How Quickly Will I Recover After Treatment?
Generally speaking, when you get therapy, your heart attack symptoms should lessen. During and for a few days following your hospital stay, you may probably experience some residual weakness and exhaustion. You will get advice from your healthcare practitioner regarding rest, medicine, and other matters.
Moreover, recovery from the therapies differs according to the therapy approach. This often requires four to five days in the hospital. The length of time you should anticipate being in the hospital is as follows:
- Patients who are given only medicine often stay in the hospital for 6 days.
- Because PCI treats a heart attack in a less intrusive way than surgery, recovery following PCI is simpler. PCI patients often remain for 4 days on average.
- Due to its substantial nature, recovery after cardiac bypass surgery takes longer. 8 to 12 days is the typical duration of stay for CABG.
When Can I Get Back To My Regular Activities?
Following discharge from the hospital, recovery from a heart attack is contingent upon the severity of the incident, the timing of treatment, the therapies received, and any pre-existing medical issues.
Your healthcare practitioner can outline what to expect and the following steps in your rehabilitation. After a heart attack, most people may usually resume their regular activities or go back to work two weeks to three months later. Heart rehabilitation can assist patients in returning to their previous level of physical activity safely and progressively.
When Should I Visit My Physician?
Following a heart attack, you are more likely to experience another one. Your doctor may likely advise follow-up treatment, testing, and monitoring to prevent more heart attacks. Among these are:
- Heart scans:
Similar to the techniques used to detect a heart attack, these can evaluate the consequences of your heart attack and identify any irreversible heart damage. They can also check for circulation and cardiac issues that raise the risk of more heart attacks.
- Stress test:
When your heart is working harder, these scans and tests might reveal any issues that could otherwise go undetected.
- Cardiac rehabilitation:
By enhancing your general well-being and way of life, these programs assist you avoid having another heart attack.
Despite being the most prevalent symptom, chest discomfort is just one of many typical indicators of a heart attack.
There are efficient therapies that can help restore blood flow to your heart and reduce consequences if the tests reveal that you’ve suffered a heart attack.
Find out more about the heart-affecting Medypharmacy website.